Dr. Jeffrey Hergenrather of Sebastopol is an OG among cannabis clinicians. He incorporated the herb into his practice back in the 1970s when he and his young family were living at The Farm, an intentional community in Tennessee. They moved to Sebastopol in 1983. Jeff, who had gone to college and medical school at Brown, would spend 26 years as an ER doc in Santa Rosa; Starr taught theatre arts and dance at Analy High School.
After California voters legalized marijuana for medical use in 1996, Hergenrather immediately began authorizing patients to use it to treat a wide variety of conditions. (All but a few doctors remained fearful for years, waiting to see what the state medical board would let them recommend it for –as if the law didn’t explicitly allow them to recommend it to treat “any condition for which marijuana provides relief.”) In the winter of 1999/2000, when Dr. Tod Mikuriya organized the group of specialists now known as the Society of Cannabis Clinicians, Hergenrather was a charter member. He served as president of the SCC from 2008 through 2018. Today there are 564 active members in 30 countries.
Although the SCC has grown over the years, the field of cannabis medicine has stalled. Crucially, only nine percent of US medical schools are now teaching students about the endocannabinoid system –the same small fraction that had added the ECS to their curricula by 2017. By that year the Legal Cannabis Industry had effectively swallowed the medical marijuana movement. My morale cracked. I had walked into the Single Issue Trap in ’96 with my eyes wide open.
I recently asked Hergenrather, who is now in his seventies, if he had any plans to retire. It’s not a realistic prospect, he said, because too many patients are relying on him. The recent retirement of Dr. Frank Lucido, an SCC charter member who saw patients in Berkeley, has added to his load. Most who seek him out need help in dealing with various cancers, agitated behaviors in dementia, autism and epilepsy (family members’ or their own). “These people are exceptionally needy,” he says. The chronic pain patients who once made up a substantial fraction of his practice now might touch base occasionally, he says, “but most can go to a dispensary and figure it out for themselves.”
I asked the obvious question: “Why aren’t there young doctors capable of treating these patients appropriately?”
Hergenrather: “My feeling is that the young doctors have never had a decent training about the endocanmnabinoid system. There may have been mention of it in a Physiology class, but we talked to an anesthesiologist from UCSF recently who said he knew nothing about the endocannibinoid system or about cannabis as medicine. It was stunning to me: that you can actually get through medical training without understanding a basic part of human physiology!
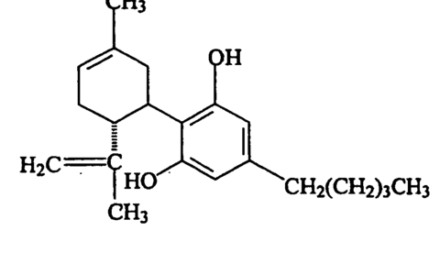
“And even if they were to learn that there is such a modulating system, they don’t get in the context of THC articulating with this system, and why it’s useful in treating such a wide range of conditions.”
After checking online Hergenrather confirmed, “According to the Association of American Medical Colleges, only nine percent of medical schools teach anything about the endocannabinoid system and how it relates to medical cannabis science… I found some cautions about the use of CBD with anti-epilepsy drugs –warfarin, amiodarone, and levothyroxine. My comment would be that even though cannabinoids and these drugs may be metabolized in the liver by the same Cytochrome P-450 pathways, the effect on drug levels is minimal under most circumstances. High CBD and clobazam (Onfi) can be problematic because its first metabolite, desclobazam, is very sedating. I don’t believe using clobazam precludes the use of CBD but dosing of both should be followed very closely with blood levels of the clobazam.
“I don’t know of other significant drug-drug interactions with these other drugs listed above.”
Who is to Blame?
In 2019 Dr. Jeffrey Block, a pro-cannabis physician based in Miami, shared these observations: “Med schools’ not teaching about the endocannabinoid system is a pernicious effect of prohibition that keeps doctors ignorant. The National Board Exams (NBME) are of crucial importance to the med schools because they are the single biggest determinant of the ranking of med school by US News & World Report.
“If you add cannabinoid medicine to the med school curriculum, you have to take something or some things out. They’re not prepared to do that because they don’t get the same bang for the buck in terms of how their students do on the national boards, because there are no questions about cannabinoid medicine.
“It comes down to money. When benefactors are deciding which endowment to contribute to, US News & World Report is very influential. Students and teachers are also influenced by the rankings in US News & World Report.
“Medical schools teach to performance on exams. This isn’t unique to medical schools, you see it in elementary schools.”
The NBME is only of the hidden valves that channel medical education —and thus the practice of medicine— in directions profitable to Big Pharma. The Federation of State Medical Boards and the Accreditation Council for Continuing Medical Education serve the drug companies’ purposes, too. These almost omnipotent bureaucracies –which we, the people know nothing – get funding and advance the interests of Big PhRMA. They are side-branches of the Deep State.
Don’t expect any exposés to come from the Soros-funded strivers who usurped control of the medical marijuana movement from Tod Mikuriya, Dennis Peron and the other authentic grass-roots leaders way back when. They’re devoting themselves to the noble cause of psychedelics.