By David Hadorn, M.D. and Linda Jackson, L.V.N. (November 2003)
ABSTRACT: Telemedicine refers to health services delivered using electronic communication media, which are used primarily to provide services to patients in rural and other underserved areas. A physician-nurse team conducted a study of telemedicine in the setting of patients seeking evaluations for possible approvals to use cannabis as medicine under California’s applicable law. Ninety-three patients were screened in-person by the nurse, including measurement of blood pressure and pulse. The physician then interviewed the patient via videoconferencing using a high-speed internet connection and real-time webcams. Patients who required in-person physician examination were referred elsewhere. Doctor, nurse, and patients were satisfied with the process. Seventy-six percent of patients (N=90; three patients did not complete the survey) felt they were able to communicate with the doctor almost as well as in person, 78 percent felt they were able to get the information they needed almost as well as in person, and 43 percent felt that having there next consultation using videoconferencing would be no different from in person; 52 percent said having their next consultation that way “would be fine”. We conclude that our teleconferencing protocol was well-suited to the provision of medical cannabis evaluations.
Introduction
The term “telemedicine” was coined in 1971 by Willemain and Mark,1 but electronic transmission of health information was first accomplished by Alexander Graham Bell in 1876 when he called to his assistant for help over the telephone after spilling acid on himself. The use of telemedicine, typically defined as “the provision of health care services, clinical information and education over a distance using telecommunication technology”2 has steadily increased over the past 30-odd years, and particularly over the past five years. There are now at least two professional associations3 4 and two peer-reviewed journals5 6 devoted exclusively to telemedicine (also called telehealth or telecare, although some observers make minor distinctions between these terms), and a recent search of amazon.com revealed 63 books on the subject of telemedicine.7
Telemedicine is usually used to provide services to patients in areas remote from medical centers and physicians. The long-distance nature of telemedicine has made it a natural outgrowth of space programs around the world, and indeed these have been instrumental in the development of this field. The National Aviation and Space Administration (NASA) provided “proof of concept” by providing a special satellite for use in disaster relief operations following the devastating earthquake in Mexico City in 1985. This linkage enabled provision of medical advice and direction, among other things, after all land-based communication had been cut off.2 A recent report from the Russian Space Agency8 details progress in the use of telemedicine in Russia and stated that “Telemedicine education and application throughout Russia has its roots in Russia’s space program.” The European Space Agency recently reported its progress in telemedicine programs, which it initiated in 1996.9
Recent articles describing the use of telemedicine have appeared in a variety of general and specialty (non-telemedicine) journals, including provision of mental health services to the elderly;10 ophthalmologic evaluation;11 12 13 management of spinal cord injury patients with pressure ulcers,14 evaluation of patients pre- and post-plastic surgery,15 and for general health, hospital, and nursing home evaluations in rural settings.16 Many more applications are described in each issue of the telemedicine journals cited above.
There are many telemedicine programs operating in California, particularly in rural and other medically underserved areas. The California Telehealth and Telemedicine Center (www.cttconline.org) administers four grant programs supporting “California organizations in developing and implementing telemedicine and telehealth projects thatprovide underserved communities with improved access to health services and health information.”
Despite these efforts, telemedicine has yet to become mainstream. A recent review concluded that although “many clinical services can be provided via telemedicine to patients who live in physician shortage areas,” major challenges remain before this technology can be more broadly accepted, including “financing, safety standards, security, and infrastructure.”17
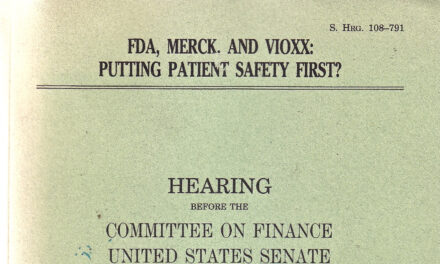
Physicians have been reluctant to embrace telemedicine, in part because of uncertainties concerning the legal and regulatory implications. A recent review of laws, regulations, court and administrative decisions, and the ethical, legal and medical literature pertaining to practice of telemedicine in the US and Europe, identified:
four main areas of concern: the doctor-patient relationship; malpractice and cross-border licensure; standards; and reimbursement. The lack of generally agreed interstate and international standards of law and ethics means that telemedicine and e-medicine will continue to struggle to gain widespread support from providers, patients and regulatory bodies as an acceptable means of health service delivery.18
We have been unable to find any mention of standards or guidelines for telemedicine in the California Medical Practice Act or in the regulations promulgated by the Medical Board of California. This leaves physicians more or less on their own to determine what constitutes appropriate use of telemedicine, based on the growing literature and their own experiences and judgment. In large part, appropriate use of telemedicine depends on the exact nature of the technology used and on the specific purpose of the encounter. Our interest was in developing a system that could be used for purposes of evaluating patients for possible recommendations or approvals of cannabis medicine, as permitted under California’s Health and Safety Code #11362.5 (Proposition 215).19
Telephone Consultations
The most common form of telemedicine is the use of the telephone to provide health advice, at times including prescriptions for pharmaceutical drugs. Although most telephone consultations probably occur in the context of a existing physician-patient relationship, this is not always the case. Indeed, physicians often provide advice (and prescriptions) for patients they have not seen and may never see, such as when physicians are “on call” for their partners.
Little formal guidance is available concerning the benefits and risks of telephone interactions, or their place in the standard of care, but a recent article in the British Medical Journal20 considered in some detail the use of the telephone for obtaining clinical information and providing medical advice. The article cited studies showing satisfactory outcomes from telephone consultation for such acute conditions as respiratory tract infection, headache, fever, cystitis, and musculoskeletal symptoms, such as low back pain. Chronic conditions, including systemic lupus erythematosis, have also been successfully managed by telephone.
The article notes that telephone consultation is often satisfactory because in a substantial majority of cases the history alone is sufficient to make the diagnosis: “In spite of advances in diagnostic procedures, eliciting the patient’s history is still the most important part of the diagnostic process. In new conditions, the final diagnosis can be reached after the history has been taken in up to three quarters of cases.” We believe this figure is even higher for chronic conditions (see below).
The article continues: “On the other hand, visual messages and non-verbal communication account for up to 55% of the impact in a face to face consultation.” Concerns about the lack of visual cues in telephone encounters was echoed in several “rapid responses” to this article (http://bmj.bmjjournals.com/cgi/eletters/326/7396/966) and we agree that it is important to actually *see* patients for their initial evaluations, in order to be able to observe cues contained in facial expressions, mannerisms and body language. This belief also rules out the use of internet “chats” for first evaluations, although both internet and telephone can probably be used safely and effectively for most cannabis-medicine re-checks).
Videoconferencing
These considerations leave videoconferencing as the only feasible telemedical modality for providing initial medical cannabis recommendations or approvals. Using this technique, it is possible to see patients “facial expressions, mannerisms, and body language as they occur, and to observe scars, limps, range of motion, and a variety of other physical signs. While auscultation, percussion, and palpation are precluded in these encounters, we believe that these diagnostic modalities play a very limited role in the evaluation of patients with chronic conditions, especially when that evaluation is focused on the appropriateness of treatment with cannabis medicines – arguably the least toxic of therapeutically active substances.
Indeed, after evaluating over 500 patients on an in-person basis in our offices in Berkeley and Oakland, California,21 we believe that very few (if any) patients require actual physical touching in order to establish a diagnosis with reasonable medical probability. The history provides the diagnosis in close to 100 percent in patients with chronic conditions, at least if they are “adequate historians”. Since almost all patients who are candidates for cannabis approvals or recommendations have chronic conditions, diagnoses can be confirmed in almost all of these patients through history alone. Patients with uncertain diagnoses or who require physical examination or testing can be (and were) referred to another physician for further evaluation.
Dr. Tod Mikuriya pioneered the videoconferencing approach to medical cannabis evaluations several years ago in patients who lived far from his office in Berkeley, California. According to personal communications, Dr. Mikuriiya considered these encounters adequate but somewhat clumsy.
Based in part on Dr. Mikuriya’s early experiences, the California Cannabis Research Medical Group,22 an ad hoc group of physicians in the San Francisco area who are active in providing cannabis-medicine approvals, have proposed that use of telemedicine be restricted to re-approvals in patients who had been seen and approved initially in person. Although we respect this view, contemporary technology provides a far superior communication experience than was available just a few years ago. Moreover, we have been very concerned that only a small number of physicians in California have been willing to provide cannabis approvals or recommendations. Development of an effective telemedicine technique could substantially increase the accessibility of patients to doctors currently active in this field, most of whom practice in the San Francisco Bay area, and could also encourage additional physicians to participate. This goal is congruent with one of the main rationales for telemedicine: permitting access to physicians for patients in underserved areas, which includes almost all of California outside the Bay area with respect to the provision of cannabis medicines to patients with chronic suffering.
The clinical safety margin offered by cannabis medicines is such that there is very little possibility of harming patients by approving continued cannabis use (almost all patients in our practice are already using cannabis for symptom relief at the time of initial evaluation). The only real clinical risk in this setting is missing the diagnosis of an acute or progressive condition, which cannabis could mask. One of us (DH) discusses the issues of safety and risk at length in a clinical practice guideline on this topic.23
Against the above background, we conducted a study to determine the feasibility and acceptability to patients of a videoconferencing approach to initial patient evaluations for medical cannabis approvals under California Health and Safety Code #11362.5.
Methods
Although the principal objective of this study was to determine the feasibility and acceptability of videoconferencing with patients in our practice, at the same time it was essential to provide patients with substantial in-person evaluation and education. This was delivered by the nurse on our team (LJ), who took patients “blood pressure and pulse, assisted with filling out the clinical intake forms, and provided comprehensive, standardized patient education, including detailed information on the advantages of non-smoked forms of cannabis medicine (e.g., tinctures).
The study was conducted August – October 2003. Patients were self-referred based on the listing of our practice on a website maintained by the California branch of the National Organization for the Reform of Marijuana Laws, through referrals by other physicians and previous patients, and through “word of mouth”.
The clinical encounter consisted of two parts. First, patients were interviewed by LJ to determine if they had a reasonable likelihood of being approved by DH for cannabis medicines under CH&S Code #11362.5. Patients typically excluded at this point included those with poorly controlled psychiatric conditions, especially schizophrenia. These patients were referred to a psychiatrist. No patients under 18 years of age were evaluated or approved, although we are aware of impressive anecdotal information that minors can benefit substantially from judicious use of cannabis medicines.24 Patients with acute or inadequately evaluated symptoms were also referred elsewhere.
Patients passing these screens were asked to sign two consent forms, the usual permission to treat form and a separate one agreeing to be interviewed by DH via videoconferencing. Patients then completed a thorough intake form covering chief complaint, history of present illness, past medical history, family history, and experience to date with cannabis as medicine. LJ assisted patients as needed and reviewed the form for accuracy and completeness. Any specific points that needed to be brought to the attention of DH were identified.
The patient was then asked to read a three-page description of alternative methods of administering cannabis; tinctures and vaporizers in particular were encouraged in order to avoid any hazards associated with smoking. A brief description was also provided concerning the legal aspects of medicinal cannabis, including the difference between State and federal laws. Patients then took a quiz covering these topics; incorrect responses were reviewed and discussed by LJ.
At this point the videoconference was initiated. LJ reviewed the patient’s intake form with DH, item-by-item, identifying any particular points that needed physician attention or review. During this recitation DH took notes of the key points, using these notes to formulate an initial approach to the interview.
The patient component of the video interview then commenced, beginning with a brief explanation of the process and proper use of the controls. DH initially welcomed patients to his “virtual office” and asked if they were able to see and hear him OK. With rare exceptions, patients responded in the affirmative and the interview was underway. A few quick initial exchanges helped to reassure the patient that he or she was being heard and responded to in real time. Also, DH made a point of nodding regularly while patients were talking in order to reinforce the real-time nature of the conversation. After a few questions and answers, almost all patients appeared to be comfortable with the technology.
Interviews were 15-20 minutes in length and covered all pertinent aspects of the present illness, history of previous work-up, residual physical or psychological symptoms, previous experiences with cannabis medicines, including any side effects experienced. (See further description of interview at url in note 19.)
Following the patient interview, LJ and DH resumed their webcam discussion, beginning with DH typing the patient’s diagnosis and any special instructions into the text-messaging area. Any other issues were then discussed, after which LJ provided final instructions to the patient (off-camera) and signed the patient’s medical record (containing the requisite approval of cannabis medicines). For this purpose she used DH’s signature stamp, which per written protocol is used only with case-by-case approval by DH following the above-described process.
Patients were asked to complete an assessment form regarding their opinions of the process. These data constitute the major outcome measure reported in this study.
At the outset of the study, a pre-test was conducted in which DH interviewed ten patients twice, once by videoconference and again in-person. After positive results were obtained on this pre-test (see below), an additional 83 patients were enrolled in the study.
Webcam Technology
After considerable research, mostly conducted on the web, we selected the iVisit software (available free from www.ivisit.com) together with a Logitech Quickcam Pro webcam (about $100). Computers at both the patient and physician ends used broadband internet connections (DSL or ADSL), with connection speeds around 1.5 megabits per second. (However, the real-time connection speed indicated in a window of the iVisit software typically read only about 50-80 kilobits per second — about the same as dial-up modem.) Our signal reliably refreshed at about 15 frames per second (FPS) using the smallest image (the highest resolution) of the three levels of resolution available. FPS dropped to about 12 using the medium image size, and to about 9 using the biggest image screen (lowest resolution). All of these were quite adequate for a real-time experience, with literally an eyeblink’s delay between the sound and visual display. FPS below 5 (as occasionally and temporarily be experienced due to fluctuations in line speed) was less satisfactory. Surprisingly, the per-second (FPS) statistic did not seem to vary based on connection speeds unless these were quite low, perhaps 30Kbps. Also, the iVisit software information indicates that broadband connections should expect an FPS figure of about 50. We never approached this figure, but were satisfied with the actual performance.
The iVisit program requires that the speaker push and hold down the “control” button on the keyboard while talking. This prevents people “talking over” each other, and incidentally prevents interruptions (which usually come from the doctor). As such, this feature is probably a benefit for the patient, although occasionally overlong answers must be tolerated by the physician and patients sometimes forgot to push the control button. (A quick reminder from DH was all that was needed in these cases, however.)
The webcam was placed as close to the screen images as possible, but there remained a distance of a few inches separation. Instinctively, patients would look at DH’s image on the computer screen, rather than the webcam, which was actually desirable as it permitted apparent eye contact when DH looked into the webcam. It was possible to maintain this “eye contact” while still frequently looking at the patient”s image by taking advantage of the periods when one naturally looks away from the other person’s eyes during conversations. In this way DH was able to see the patient quite well, including picking up non-verbal cues.
The webcam’s built-in microphone was sensitive to background noise, so in busy clinic environments or where ambient noise is significant, a headset and directional microphone were used.
Results
Overall, both DH and LJ were quite satisfied with the performance of the technology and with the assessment protocol described above. Neither of us felt unduly restricted or uncomfortable with the level and quality of information obtained and imparted during the process. Although internet or computer glitches disrupted communication on a few occasions, these were typically short-lived and surmountable.
Responses to the patient surveys of the 10 patients seen during the pre-test were positive, encouraging us to enroll additional patients (N=83) for a total sample of 93 patients. Three patients in the main part of the study did not complete the survey, leaving a total of 90 completed records.
The survey questions and responses were:
1. Using the webcam arrangement, I was able to communicate with the doctor:
Pre-Test Remaining Total
a. Almost as well as in person 8 (80%) 60 (75%) 68 (76%)
b. Pretty well, not bad at all 2 (20%) 18 (22%) 20 (22%)
c. OK, but not that great 0 2 (3%) 2 (2%)
d. Not very well at all 0 0
2. How well were you able to get the information you need?
Pre-Test Remaining Total
a. Almost as well as in person 6 (60%) 64 (80%) 70 (78%)
b. Pretty well, not bad at all 3 (30%) 15 (19%) 18 (20%)
c. OK, but not that great 1 (10%) 1 (1%) 2 (2%)
d. Not very well at all 0 0
3. How would you feel about having your next consultation done like this?
Pre-Test Remaining Total
a. No different from in person 3 (30%) 36 (45%) 39 (43%)
b. That would be fine 7 (70%) 40 (50%) 47 (52%)
c. OK, but not that great 0 4 (5%) 4 (5%)
d. Wouldn’t like it at all 0 0
4. How would you compare the in-person interview and the webcam interview (pre-test only)?
a. I got a lot more out of the in-person interview 2 (20%)
b. I got something more out of the in-person interview 2 (20%)
c. About the same 6 (60%)
d. I got something more out of the webcam interview 0
e. I got a lot more out of the webcam interview 0
In addition, we received many informal comments concerning the process, almost all of which were favorable. Typical were “this is the future of medicine” and “it seemed so space age; it was really cool”. However, a handful of patients said they missed seeing the doctor in person. Clearly, this technology would not be preferred by all patients, although everyone seemed satisfied with the level of information they received. Many patients commented that the length of time spent with DH was substantially more than the 5-10 minute physician visits to which they have become accustomed.
Discussion
Most patients shared our belief that the combination of in-person evaluation and education by an experienced nurse and a webcam interview by a knowledgeable physician was an acceptable and effective means for obtaining and imparting necessary information in the context of cannabis-medicine evaluations. It is difficult to say whether and to what extent our positive results would be experienced by other nurse-physician teams, because much probably depends on personality — not all nurses will wish to operate as autonomously as LJ and not every physician will feel comfortable using a webcam or be able to project well over this medium.
To the best of our knowledge, the form of telemedicine that we have described is fully congruent with existing standards of telemedical practice within California, and indeed within the United States and the world. Although few explicit standards have been developed in this area, we believe that our combination of nurse-in-person and doctor-via-webcam worked well.
The successful use of videoconferencing in this context could encourage many doctors, particularly retired physicians, to consider taking up cannabis-medicine evaluations as a part-time practice. This could be a boon for the millions of patients with chronic pain for whom standard pharmaceutical remedies have proven ineffective.25
In our view, the only significant objection likely to be raised against our protocol is that the lack of the physician’s physical presence (and consequent inability to physically touch the patient) could lead to mis-diagnoses and inappropriate care plans, including potentially harmful continuance of cannabis medicines. However, as discussed above, we believe it is rarely necessary to physically touch a patient in order to ascertain with reasonable medical probability whether or not they are likely to benefit (or to continue to benefit) from cannabis as medicine. Physicians evaluating patients in this setting need not attempt to stage a diagnostic coup, nor need they probe or palpate patients in search of grimaces or groans that might somehow validate the patient’s history. Such physical findings are notoriously poor indicators of diagnosis, in any case, and it would certainly be inappropriate to conclude from a patient’s “inadequate” grimace, for example, that the patient does not have “sufficient” pain to warrant the use of cannabis.
Nevertheless, physicians in this setting must, as always, be alert for clinical histories that could be indicative of acute, progressive, or inadequately evaluated problems. Such patients should be referred for further evaluation by local practitioners. This topic is discussed at length in the above-referenced guideline (note 19).
Various aspects of our process could perhaps be improved. At some point, for example, we may create an electronic medical record, which would permit e-mailing the patient intake form to DH, obviating the need for LJ to read it aloud. However, the current process has the advantage of ensuring that each item on the form is completed before being communicated to DH. We have also considered faxing the hard-copy intake forms to DH, but decided against this for financial and logistical reasons.
Our results are similar to those reported last year by Blue Cross of California State Sponsored Programs, which analyzed data from 24 primary care sites in 18 California counties, covering 27 specialities. 26:
The responses to the questionnaires indicated that telemedicine made it easier for patients to receive specialty care (91% of patients satisfied, mean score 4.6 [out of 5 possible]). There was general satisfaction with telemedicine (87%, mean 4.5), a willingness to continue receiving services (90%, mean 4.6) and most patients felt that they would not receive better care in person (61%, mean 2.3). Patients stated that they received the necessary information from specialists (85%, mean 4.5) and had their questions answered by a primary care provider or nurse (89%, mean 4.7). . . . The present study suggests that telemedicine is acceptable to patients as a method of improving access to specialty expertise, and compares favourably with face-to-face care.
The principal conclusion of our study is that telemedicine, as we have applied it, appears well-suited to the practice of cannabis therapeutics. We encourage other physicians and nurses to consider attempting to replicate our study.
————————————————————————
Footnotes
1. Willemain TR, Mark RG: Models of remote health systems, Biomedical Sciences Instrumentation 8: 9-17, 1971.
2. Maheu M, Whitten P, Allen A. E-health, Telehealth, and Telemedicine: A Guide to Startup and Success. Jossey-Bass 2001
3. Association of Telehealth Service Providers; www.atsp.org
4. American Telemedicine Association; www.atmeda.org
5. Journal of Telemedicine and Telecare; www.coh.uq.edu.au/jtt/
6. Telemedicine Journal and E-Health; www.liebertpub.com/tmj/default1.asp
7. Including:
Maheu M, Whitten P, Allen A. E-health, Telehealth, and Telemedicine: A Guide to Startup and Success. Jossey-Bass 2001
Darkins AW, Cary MA. Telemedicine and Telehealth: Principles, Policies, Performance and Pitfalls. Springer Pub Co. 2000.
Norris AC. Essentials of Telemedicine and Telecare. John Wiley & Sons, 2002.
8. Doarn CR, Lavrentyev VA, Orlov OI, Nicogossian AE, Grigoriev AI, Ferguson EW, Merrell RC. Evolution of telemedicine in Russia: The influence of the Space Program on modern telemedicine programs. Telemed J and e-Health 1993; 9: 103-109.
9. Feliciani F. Medical care from space: telemedicine. ESA Bull 2003; 114: 54-59.
10. Mitka M. Telemedicine Eyed for Mental Health Services: Approach Could Widen Access for Older Patients. JAMA.2003; 290: 1842-1843. (Medical News)
11. Editorial. Current state and future direction of tele-ophthalmology in Canada: first Canadian ophthalmic telemedicine symposium. Can J Ophthalmolo 2003; 38: 349-351.
12. Burnier MN, Telemedicine and tele-ophthalmology. Can J Ophthalmol 2003; 38: 343, 345.
13. Bowman RJ, Kennedy C, Kirwan JF, Sze P, Murdoch IE. Reliabilitiy of telemedicine for diagnosiing and managing eye problems in accident and emergency departments. Eye 2003; 17: 743-746.
14. Lewis M, Choi H, Boushell M, Barsanti P, Alquist M, Sabharwal S. Use of telemedicine in the management of spinal cord injury patients with pressure ulcers. Arch Phys Med Rehabil 2003; 84: E37.
15. Sclafani AP. Telemedicine in plastic surgery. Plast Reconstr Surg 2003; 112: 936.
16. Armer JM. A case study of the use of telemedicine by advanced practice nurses in rural Missouri. J Contin Educ Nurs 2003; 34: 226-233.
17. Myers MR. Telemedicine: an emerging health care technology. Health Care Manag 2003: 22: 219-223.
18. Silverman RD. Current legal and ethical concerns in telemedicine and e-medicine. J Telemed Telecare 2003; Suppl 1: S67-69.
19. See davidhadorn.com/cannabis/CM_guideline.htm for a discussion of clinical and legal issues surrounding such evaluations.
20. Car J, Sheikh A. Telephone consultations. BMJ 2003;326:966-969.
21. For a report describing our first 487 patients, see davidhadorn.com/cannabis/patientreports.htm.
22. www.ccrmg.org
23. See url at Note 19, above.
24. See for example Jeffries D et al.. Jeffrey’s Journey. Rocklin, CA: LP Chronicles, 2003.
25. For a good overview of the problem of physicians “under-treatment” of pain and the US government’s actions against pain-management doctors, see painreliefnetwork.org.
26. Brown-Connolly NE. Patient satisfaction with telemedical access to specialty services in rural California . J Telemed Telecare. 2002;8 Suppl 2:7-10.