By Jeffrey Hergenrather, MD —O’Shaughnessy’s 2007 editorial
In many pharmaceutical advertisements these days, a sophisticated voice on TV tells us to ask our doctors if some new drug is right for us. The drug may be designed to treat pain, insomnia, restless leg syndrome, depression, heartburn —almost any ailment to which our bodies and minds are subject. I sometimes imagine the voice intoning, “Ask your doctor if cannabis is right for you,” and wonder what the effect would be.
Even 10 years after the voters of California legalized it for medical use, cannabis has not found a place in the curriculum.
Unfortunately, most doctors would be unwilling and/or unable to answer a patient asking if his or her condition(s) might be treated effectively by cannabis. We older doctors learned little or nothing about cannabis in medical school, and even 10 years after the voters of California legalized it for medical use, cannabis has not found a respectable place in the medical school curriculum. This will change, inevitably, thanks to new discoveries about the receptor system affected by THC and other active ingredients in cannabis. (We now know that the body makes its own cannabinoids — “endocannabinoids”— that activate this same receptor system. It is impossible to teach physiology or pharmacology thoroughly without reference to the endocannabinoid system.)
The information your physician has about cannabis may have come from “findings” issued periodically by the federal government and transmitted by the media. These politically motivated reports typically exaggerate alleged dangers of cannabis. They are biased and unsubstantiated, better described as propaganda.
Fear is another deterrent to physicians discussing and approving cannabis use by their patients. Although a federal court ruling in the Conant v. Walters case clearly and permanently established the right of doctors to discuss and recommend cannabis, the Medical Board of California has investigated many for doing so. Several investigations have resulted in prosecution by the Attorney General and doctors being placed on probation. These results are duly noted in the Board’s newsletter, which every licensed physician receives. Even the doctors who are investigated but not prosecuted have to endure significant expense and protracted fear. Most doctors would rather avoid placing their licenses at risk.
The prevailing fear is reinforced by medical specialty societies such as the American Academy of Opthalmology that advise members to avoid involvement.
Patients, too, are afraid to ask their doctors about cannabis for fear of rejection and/or embarassment. This is not paranoia —some doctors reportedly refuse to treat cannabis users, or stop prescribing certain medications because they consider the inquiring patient a potential drug addict. The result of a patient who uses cannabis concealing it from his or her doctor is a relationship that is less than open and honest. For those patients who don’t use cannabis but have heard that it might be helpful, reluctance to ask their doctor might adversely affect their well-being. Everyone suffers —the patient denied access to a potentially helpful medicine, and the doctor denied information about it.
As a practicing physician, most of what I’ve learned about medicinal cannabis has come from my patients using it to alleviate their symptoms and treat their conditions.
As a practicing physician, most of what I’ve learned about medicinal cannabis has come from my patients using it to alleviate their symptoms and treat their conditions. Over the past decade, as I famliarized myself with the medical literature and began attending conferences on cannabis therapeutics, I’ve heard the benefits reported by my patients substantiated. The evolving scientific findings help explain why cannabis relieves such a wide range of symptoms: it modulates and affects many bodily processes. Ironically, much of the groundbreaking research on cannabis has been funded by the National Institute of Drug Abuse (NIDA) in hopes of finding adverse effects.
Should you ask your doctor about cannabis? Nobody knows your medical history better than the doctor who has been following you, and the ideal answer is “yes.” If you are already using cannabis —whether or not you define your use as
“medical”— the ideal answer, again, is “yes.” But in real-world terms, the answer will vary depending on your level of trust, your self-confidence, your urgency of need, your sense of your doctor’s open-mindedness, and other factors.
If you find yourself unwilling to broach the subject of cannabis, you should consider consulting a specialist. The Society of Cannabis Clinicians includes doctors who take an extensive history and conduct a complete physical exam, i.e., who treat the whole patient. Others may only take vital signs and conduct a cursory history to establish that the patient has a bona fide medical condition that he or she has been treating effectively with cannabis. Patients seeing doctors with the latter approach should also have a doctor or clinic they can go to for problems beyond the scope of the cannabis consultation.
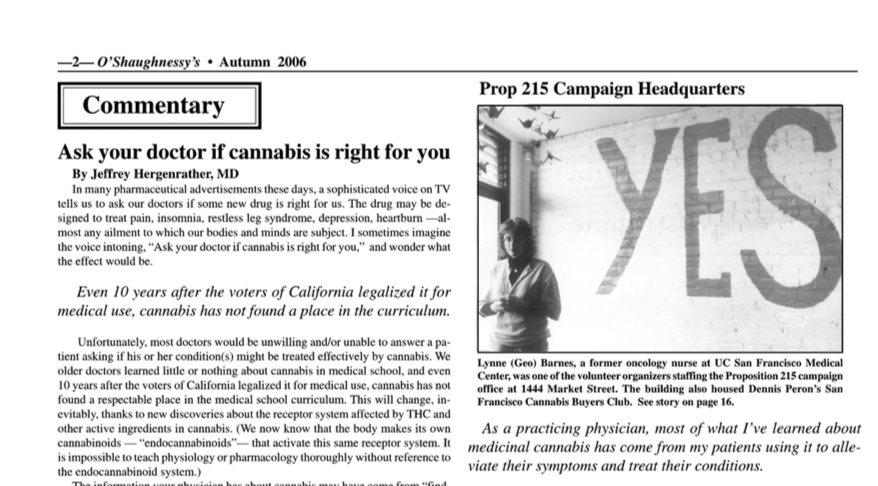
The cannabis specialists came into existence precisely because the vast majority of California doctors remained unwilling —despite the passage of Prop 215 and the Conant ruling— to approve cannabis use by patients whose conditions were other than terminal. Tod Mikuriya, MD, described himself in 1996 as “the doctor of last resort” for cannabis-using patients who didn’t want to seek approval from —or had been turned down by— their regular doctors. Over the years, as we’ve learned more about the versatility of cannabis and its mechanism of action, the cannabis consultants have gained useful expertise. Although we continue to be investigated by the medical board, the truth is, there are aspects of medicine that we understand better than our colleagues to whom the endocannabinoid system is only a rumor.
Note from the Managing Editor:
Two examples of Dr. Hergenrather’s point made national news as this issue was being prepared for publication. In late September, The Wall St. Journal revealed that Constance Gee, the wife of Vanderbilt University’s chancellor, uses cannabis to treat the symptoms of an inner-ear problem, Mrs. Gee then discussed her situation frankly with reporters from Nashville’s major daily, The Tennesseean. She has Meniere’s disease, which can cause vertigo, nausea, and hearing loss. The Tennesseean reporters contacted a supposed expert, Timothy Hullar of Washington University School of Medicine (“one of two major centers of study on Meniere’s”), who, they reported, had “never heard of anyone using medical marijuana to treat symptoms of Meniere’s.” Hullar was quoted saying “I can’t imagine going to the extreme of marijuana.”
Knowledgable California doctors routinely approve the use of cannabis by Meniere’s patients who say that it helps ease their symptoms. “Meniere’s causes dizziness, dizziness causes nausea, cannabis relieves nausea,” says David Bearman, MD. “I wouldn’t be surprised if the symptoms caused Mrs. Gee to be a little depressed —and of course cannabis helps that, too.”
Robert Sullivan, MD, corroborates: “I’ve issued many recommendations for Meneire’s, as well as tinnitus [ringing in the ears]. It works well enough to make a significant improvement in patients’ lives, i.e., symptoms not gone but much abated so they can function and carry on their daily activities, instead of sitting and suffering. It also aids sleep.”
R. Stephen Ellis, MD, of San Francsico, has given some thought to how cannabis might help in the treatment of Meniere’s. “Three possible mechanisms come to mind,” he says. “Number one, the anti-anxiety effect of cannabis would be very useful to a Meniere’s patient. These people are anxious as can be when they hit the ER. When they get an attack it’s as if they are wired —that’s why Ativan is one of the treatments, to bring them down. Two would be the anti-nausea effect. Duh! You’re barfing and there’s a drug that offers relief in 10 seconds. The third is slowing down the vertigo itself —the sensation of spinning caused by the inner ear problem. My patients say cannabis is as good as Antivert, which is the classic treatment, or Benadryl, which is used in certain situations. I recall reading that the auditory nerve does have CB1 receptors. I don’t know about the cochlear structure itself.”
In mid-October the New England Journal of Medicine published a study showing that Seroquel, Risperdal and Zyprexa, three “atypical antipsychotics” widely prescribed for Alzheimer’s patients are ineffective and cause severe adverse side effects. The study was funded by the National Institute of Mental Health, whose director, Thomas R. Insel, commented, “We need to come up with better medications.” Indeed —more than 4.5 million Americans have been diagnosed with Alzheimer’s, its environmental causes remain unknown, and it is occurring with increasing frequency.
The U.S. now has a two-tier system of medical expertise.
Is the director of NIMH unaware that rage and irritability associated with Alzheimer’s are among the symptoms alleviated by cannabis? Probably. The U.S. now has a two-tier system of medical expertise. There are doctors who have some understanding of the endocannabinoid system and the effects of cannabinoid drugs on various symptoms and conditions; and there are doctors who have no such understanding.
If you are presently using cannabis —whether or not you define your use as medical—or are considering using it for medical purposes, of course you should ask your doctor if cannabis is right for you. And if you are unable to have that conversation forthrightly, consider seeing a cannabis specialist.
From O’Shaughnessy’s Summer 2007