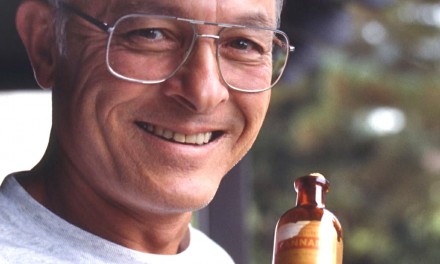
Sue Sisley, MD, is an assistant professor of internal medicine and psychiatry at the University of Arizona medical school, and a psychiatrist in private practice in Scottsdale. She has designed —and gotten FDA approval to conduct— an “Investigation of the Safety and Efficacy of Medical Marijuana in Veterans with Chronic, Treatment-Resistant Post-traumatic Stress Disorder.”
Such a study is called for, Sisley states, because “PTSD plagues between six and 10% of the US population at some point during their lifetime. A significant percentage of PTSD patients fail to respond adequately to FDA-approved treatments such as Zoloft and Paxil —suggesting a need to develop innovative treatments.”
A new treatment would be especially timely, she adds, because one in five soldiers returning from combat in Iraq and Afghanistan will have PTSD.
The Multidisciplinary Association for Psychedelic Studies raised $10,000 to support Sisley’s project and intends to raise more. Her plan is to enroll 50 veterans with “PTSD arising from their service in the US armed forces” and to assess their responses to marijuana of varying potency, including one CBD-rich strain. Participants will be men and women 18 or older with a diagnosis of PTSD that has not improved after medication or psychotherapy.
The investigation Sisley proposes seems small, simple, and short-term.
In the first stage (four weeks) groups of 10 patients each will use marijuana of varying potencies—0% THC, 2% THC, 6% THC, 12% THC, and 6% THC plus 6% CBD. Their daily dose will be 1.8 grams. Within each group, half will smoke pre-rolled cigarettes, half will vaporize.
In the second stage (also four weeks), to begin after two weeks of abstinence, participants will be divided into three groups —20 using 6% THC, 10 using 12% THC, and 20 using the CBD-THC combo. In each group, again, half will smoke and half will vaporize the 1.8 gram daily dose.
Perceived effects will be reported by subjects to the investigators daily by phone during the first week of each stage, and at weekly meetings.
CBD in the mix
Sisley puts forth three hypotheses:• “Marijuana will ease the symptoms of PTSD, specifically reducing nightmares, improving sleep, and improving mood as measured by the Clinician Administered PTSD scale (CAPS)” and other evaluation methods.• “Marijuana, in a dose dependent manner, will ease the symptoms of PTSD.
• “Marijuana with 6%THC and 6% CBD will be more effective than marijuana with 6% THC alone.”
Sisley and MAPS have been getting the runaround from the federal government. The Food and Drug Administration (FDA) approved Sisley’s study protocol in April 2011. But it was rejected in September by a review committee from the National Institute on Drug Abuse and the Public Health Service (NIDA and PHS, which are part of Health and Human Services).
The rejection letter contained four put-downs. The first was personal: “While Dr. Sisley’s CV indicates that she is an experienced clinician, she lacks sufficient research expertise.” (When the name of the game is Science, freshmen can’t play for the varsity.)
Secondly, the study design was deemed too “complex” and “a simpler design might be preferable for this pilot study.”
Third, the experts criticized the study because it did not “provide a basis for determining individual differences in efficacy” —which contradicts the call for a simpler design.
Finally, “A number of safety concerns were raised. Some reviewers were concerned about the use of drug-naive participants. Documentation of an IRB review was not submitted.” (In October 2012 the University of Arizona Institutional Review Board approved Sisley’s protocol, removing that particular hurdle.)
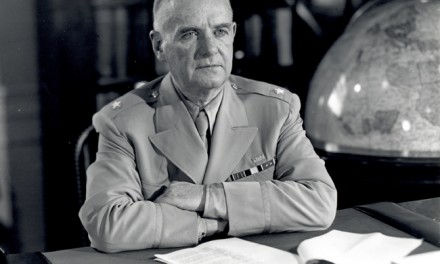
“Marijuana is the only Schedule 1 drug for which the federal government not only controls the supply, but also requires a special review of all scientific protocols by a NIDA/Public Health Service (PHS) review panel,” observes Rick Doblin of MAPS, who has spent more than a decade fighting federal bureaucrats on behalf of Lyle Craker, a UMass Amherst botany professor who wants to grow marijuana for research purposes.
With no herb legally available to provide to patients, Sisley’s PTSD study remains in limbo. “Until,” says the ever-hopeful Doblin, “NIDA agrees to sell our researchers the marijuana, until MAPS succeeds in growing its own marijuana for research, or until the marijuana can be legally imported.”
Arizona’s neighboring state, New Mexico, specifically acknowledges PTSD as a condition that can be treated by marijuana. As of February 2013, 3,467 patients had been authorized by doctors to medicate with it —out of 8,263 patients authorized overall. The high percentage of New Mexicans with PTSD diagnoses using cannabis indicates that it is one of the conditions for which the herb is most beneficial.
Background: UMass Seeks License to Cultivate