Fear makes labor last longer, according to a Norwegian study published in 2012. A team led by Samantha Salvesen Adams at Altershus University Hospital constructed a fear-of-childbirth scale based on a 33-item questionnaire given to 2,206 women who were eight months pregnant. (The researchers eliminated those carrying twins, breech presentation, and elective Caesareans.) Women in the upper half of the fear scale had an average labor 47 minutes longer than those in the lower half. “Stressed women have higher stress hormones during pregnancy, and high stress hormones may weaken the power of the uterus to contract,” according to Adams.
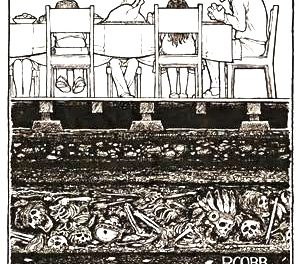
No peer-reviewed study has looked at whether cannabis use during pregnancy would reduce stress-hormone levels and lead to speedier delivery. The conventional wisdom of the medical establishment —enforced by Child Protective Services— is that cannabis use by pregnant women will endanger their offspring. This conventional wisdom is based on some of the phoniest studies ever funded by the National Institute of Drug Abuse, and has been thoroughly refuted by Melanie Dreher, Dean of Nursing at Rush University Medical Center in Chicago. (See O’Shaughnessy’s summary of Dreher’s findings here.)
We came across the Norwegian study about the impact of fear in researching a question posed by attorney Jennifer Ani to analytic chemist Don Land of Steep Hill/Halent Lab. Ani wrote:
“I have a client who used cannabis pursuant to her recommendation until she learned she was pregnant, 12 weeks into the pregnancy. DCFS is threatening removal because cannabis was found in the child’s meconium, although they’ve not produced that test despite my request.
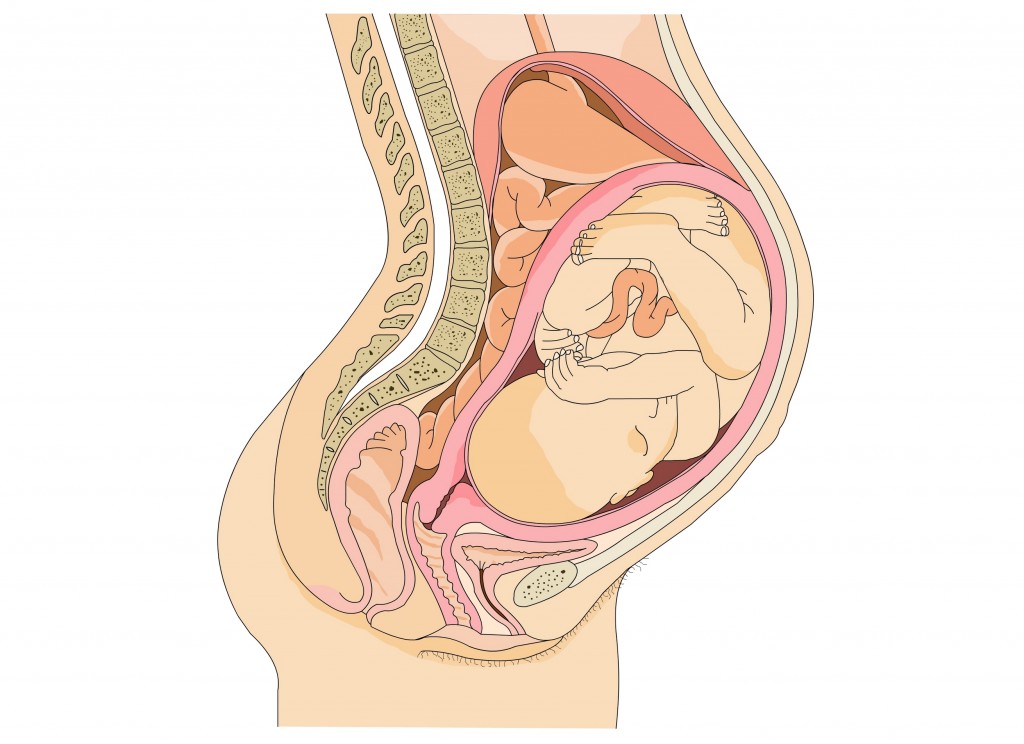
“Do you think that you could give me a declaration on meconium [the baby’s first poop, containing material ingested before birth], specifically, the fact that, if a woman used cannabis until the 12th week of her pregnancy and then quit, that it would logically be present in the child’s meconium at birth? Also, do you have any thoughts on what was actually transferred to the fetus, as far as the content of the cannabis or the breakdown of it?
Dr. Land replied:
I have found very little. This reference from 2011 (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3163087/) shows results for twenty meconium samples that tested positive for cannabinoids or their metabolites (Table 2) out of a total of 86 pregnant women, 38 of which self-reported cannabis use at some point during pregnancy (i.e., half of pregnant users resulted in no positive results in meconium). Self-reporting and oral fluids testing at each trimester were used to verify use/abstinence throughout the study. Of the twenty positives, two were from infants whose mothers stopped using in the first trimester and one was from a woman who self-reported as not using. For all three, very low levels (below 20 ng/g) of THCCOOH were detected in the meconium. Much higher levels were found in some users who report continued use into the 2nd and 3rd trimesters, but some others of those were also very low.(By the way, I do not believe these authors did their statistical analysis correctly on their major findings —that there were differences in size and weight for cannabis use— their conclusions about discernible differences do not seem to match the numbers they report.)I have read that meconium starts forming at 12-16 weeks and is not subject to metabolism, so any levels of THC or metabolites in the mother at that point could lead to detectable levels in meconium, theoretically…we don’t yet know what levels were detected in this case.
I had two cannabis babies in the early seventies and know of countless others and pregnancies that were normal and deliveries that were normal and babies that thrived and grew and developed normally into adulthood—normal in the sense of statistical comparison with others who did not use during pregnancy. No sense of cannabis toxicity!