Daily Marijuana Use is Not Associated with Brain Morphometric Measures in Adolescents or Adults.
This headline was the title of a paper published in the Journal of Neuroscience January 28, 2015, and our nominee for Downplayed Study of the Year. Barbara J. Weiland and colleagues at the University of Colorado and the University of Louisville found that marijuana use does not cause lasting measurable changes in the brain. (Morphometrics pertains to the measurement of shape.)
This is almost a Tashkin-level exposé. (UCLA pulmonologist Donald Tashkin and colleagues reported in 2005 that smoking marijuana does not cause lung cancer.) And just as Tashkin’s findings were buried by the biomedical establishment and corporate media, so, too, has the study by Weiland et al.
Reviewing the papers purporting to show that marijuana use alters brain morphology, the authors found serious inconsistencies—“Marijuana use has been associated with both increased (Cousijn et al., 2012) and decreased (Yücel et al., 2008; Demirakca et al., 2011; Solowij et al., 2011) volumes of subcortical structures, or both (Battistella et al., 2014).”
The influential studies also have a serious limitation: “Importantly, these studies were not designed to determine causality (i.e., that marijuana use causes morphological changes), which would require a longitudinal design to establish temporal precedence.”
Moreover, the conventional wisdom is based on studies that “did not adequately exclude the effects of confounding variables. Several reports included marijuana groups that differed from control groups in alcohol use/abuse (Demirakca et al., 2011; Solowij et al., 2011; Schacht et al., 2012; Gilman et al., 2014). Unlike marijuana, alcohol abuse has been unequivocally associated with deleterious effects on brain morphology and cognition in both adults (Sullivan, 2007; Harper, 2009) and adolescents (Nagel et al., 2005; Medina et al., 2008; Squeglia et al., 2012). Statistically controlling for comorbid alcohol abuse, as many studies do, is not an ideal strategy, especially in small groups or under conditions where covariates may interact with the independent variable (Miller and Chapman, 2001). Thus, it is possible that alcohol use, or other factors, may explain some of the contradictory findings to date.”
Weiland et al did brain scans on 29 adult daily users and 50 adolescent daily users, and an equal number of non-users (controlling for age, sex, etc.), and looked for changes. “We evaluated the following structures that were the focus of recent studies of marijuana: the bilateral nucleus accumbens and amygdala (Gilman et al., 2014); hippocampus (Demirakca et al., 2011; Schacht et al., 2012); and cerebellum (Solowij et al., 2011; Cousijn et al., 2012).”
The studies reporting brain damage have all been widely publicized by the mass media and accepted as Scientific Truth. For example, the New York Times ballyhooed Gilman’s findings in an October 29, 2014 article wittily headlined, “This is Your Brain on Drugs.”
Times reporter Abigail Sullivan Moore visited Dr. Jodi Gilman at the Harvard Center for Addiction Medicine and rhapsodized: “The gray matter of the nucleus accumbens, the walnut-shaped pleasure center of the brain, was glowing like a flame, showing a notable increase in density,” as Dr. Gilman explained what addiction looks like on a computer screen.
Moore of the Times was hooked: “Even in the seven participants who smoked only once or twice a week, there was evidence of structural differences in two significant regions of the brain. The more the subjects smoked, the greater the differences.”
The self-styled “paper of record” ignored the study by Weiland et al, although, as the authors note matter-of-factly, “The analyses we performed duplicated those previously used (Gilman et al., 2014) with several important differences.
“Our study included more subjects in adult and adolescent samples, and compared extreme groups of non-marijuana users to daily users.
“Most importantly, the groups were closely matched on an alcohol problem measure (AUDIT) and were not different on many possible confounding variables (e.g., tobacco use, depression, impulsivity, age, and gender).
“In other words, the present analyses had greater power to detect group differences, while closely controlling for other effects.
“We found no evidence of differences in volumes of the accumbens, amygdala, hippocampus, or cerebellum between daily versus nonusers, in adults or adolescents.
“Moreover, effect size data suggest that potential effects are modest and would require very large sample sizes to detect significant differences.
“The lack of significant differences between marijuana users and control subjects in the present study is consistent with the observation that the mean effect size across previously published studies suggests no clear effect of marijuana on gray matter volumes.”
The new phrenology
“The new phrenology,” is a term Tod Mikuriya, MD, used to describe studies showing marijuana use causing changes in the brain. Although structural changes would be worrisome, Mikuriya said, it would still have to be shown that those changes result in adverse cognitive or behavioral changes. Weiland et al make the same point:
“It is also unclear how variations in the morphology of cortical or subcortical structures would be interpreted. For example, others have interpreted reductions of gray matter volume in the accumbens as evidence of the deleterious effects of alcohol (Makris et al., 2008), yet increases in accumbens volume associated with marijuana use were interpreted as deleterious (Gilman et al., 2014).
“Future research should link structural differences to behavioral or functional measures to better understand the implications of differences in brain morphology. In addition, the morphological techniques used for analyses show substantial variation in results depending on processing and software, particularly shape analysis (Gao et al., 2014).”
What will get taught?
When we first dummied this issue of O’Shaughnessy’s, the editorial was going to be a demand —the same demand we’ve been making since the first issue in 2003—that Cannabis-based Medicine be added to the medical school curriculum.
But we came to see how inadequate that demand is. The endocannabinoid system is about to be added to the curriculum. The MCPHS class described by Matt Metcalf is surely a harbinger of many more to come in the era of quasi-legalization.
The key question is: who will determine the content? Metcalf declares, “The entire course is based on what the primary, peer-reviewed, research literature has revealed about medical applications for cannabis and drugs targeting the endocannabinoid receptor system.”
But Barbara Weiland’s powerful critique of the primary, peer-reviewed research literature based on neuroimaging reminds us how unscientific that literature actually is.
We also intended to join the chorus of praise for Sanjay Gupta. His “Weed” Specials on CNN brought cannabidiol to the attention of the American people, and he acknowledged having been systematically miseducated on the subject of marijuana. Grateful that Gupta publicized Charlotte Figi’s improvement, we downplayed the signficance of his homage to Dr. Staci Gruber at McLean’s Hospital (New England headquarters of the psychiatric establishment, a subsidiary of Big PhRMA).
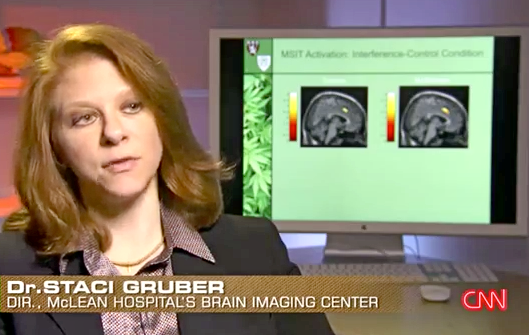
Dr. Gruber, the director of McLean’s Brain Imaging Center, is a PhD, not a medical doctor. Here’s the script:
Gupta (as if awed): She’s using high-tech imaging to see what happens in the brain when you smoke.
Gruber: What we see is a very big difference in people who begin to smoke prior to the age of 16 and those who smoke after age 16. What we call “early” versus “later onset.”
Gupta: Gruber’s brain scans show that the white matter —those are the high waves that help the brain communicate from one point to another— are impaired in those who start smoking early.
Gruber: Maybe that there’s underlying white-matter-conductivity differences.
Gupta: Those white matter highways are just more disrupted in people who start smoking early.
Gruber: That’s what we see.
Gupta: Perhaps not surprising given what we know about the young developing brain.
Preliminary research shows that early-onset smokers are slower at tasks, have lower IQ’s later in life, higher risk of strokes, and increased incidence of psychotic disorders. And while these studies are not conclusive, some scientists are still concerned because in 2012, 35 percent of high school seniors lit up, and that could mean a generation of kids with damaged brains. And many fear something else.Cut to a teenager identified in the CNN transcript as “Joel Vargas, Addicted to Marijuana.” Joel tells Gupta, “I never really told myself I need help.” We wonder who really told him. Possibly dear old mom and dad.
Gupta: A generation of marijuana addicts. When we come back, the truth and the science behind what’s being called a growing epidemic…
Gupta does not make good on his bold claim. ”In fact,” he said authoritatively when we came back, “nine percent of marijuana users will become dependent. Now that’s not as high as other drugs, like heroin —23 percent of users become addicted— or 17 percent with cocaine, 15 percent with alcohol. But it’s still approximately one out of every 11 marijuana smokers.” This deceptive riff is reenforced by an accompanying bar graph. 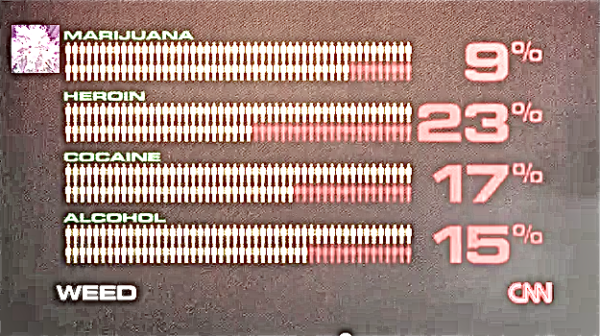
There’s nothing like a specific number to make an assertion seem like a fact. The “9-percent-become-addicted” line has been put out by the National Institute on Drug Abuse since the 1990s. It is supposedly substantiated by the number of people in marijuana treatment programs. But very few people go into treatment because they think they are impaired by marijuana. Most go because they’ve been forced to by a judge, an employer, a school, or a parent. For many so-called marijuana addicts who use the herb for pain or insomnia and go to work unimpaired, the real “problem” is the metabolite level detected in their urine. For depressed teenagers the real problem is the situation and/or environment they find so unbearable that they want to alter their consciousness every day.