By Frank H. Lucido, MD, with Mariavittoria Mangini, PhD, FNP
from O’Shaughnessy’s, Spring 2004
Clinical medicine, as I have experienced it during a quarter century of practice, is a constantly evolving system. Every practitioner has a different approach to gathering clinical information, diagnostic reasoning and therapeutic decision making. There is rarely a single correct way to care for patients. Instead, there is usually a wide variety of acceptable approaches, any of which may be appropriate in a given situation1. (Goldberg, 2002b).
Particularly for the student, but also for the experienced clinician working to incorporate a new technique or finding into his or her established practice, the array of choices may be disconcerting and may provoke a feeling of reluctance to enter into unfamiliar clinical territory.
The use of medical cannabis to provide symptom relief to seriously ill patients is a practice that has been rediscovered and refined following the 1996 passage of the California Compassionate Use Act (“Proposition 215,” which became Section 11362.5 of the state Health and Safety Code).
A Medico-Legal Consultation
After the passage of Proposition 215, I began performing cannabis evaluations on a very limited number of my existing primary care patients, who requested it and whom I knew had clear indications such as nausea of cancer chemotherapy, severe migraine headache, and chronic pain.
Soon I was receiving referrals for medical cannabis evaluations for patients I had not seen before. These referrals came from both patients and other health care providers. This is not surprising, since most doctors are reluctant to approve medical cannabis. Most physicians don’t know the law, and have never studied the medicinal uses and history of cannabis. Medical schools do not teach about cannabis’ potential benefits, medicinal uses and history. When this lack of information is added to concerns that many health care providers have about the legal and professional implications of cannabis recommendation, it is understandable that a minority of doctors are doing the majority of evaluations on cannabis patients.
As I began seeing more patients who were benefiting in a wide variety of ways, it became clear to me that I had to become better acquainted with the professional literature on cannabis as a medicine.
To the extent that my general primary care practice is typical, I would guess that most general primary care practices in the Bay Area have seriously ill patients likely to benefit from the use of medical cannabis. Possible benefits might include improved symptom relief, fewer side effects, and/or lower cost than many commonly prescribed pharmaceuticals.
What is not typical about my practice is that even among the limited number of doctors who are performing medical cannabis evaluations, I am one of the few who does them in the context of a full-scope general medical practice.
So, for more than seven years, I have been conducting medico-legal consultations for patients who are weighing cannabis as a treatment option. I have worked to develop my own standards by reading the scientific literature, learning from the experience of other practitioners, and through application of my past experience in making clinical decisions.
In describing my own approach, I in no way intend to define the standard that is appropriate for all providers or all clinical situations. Rather, this article represents the accumulated insights from my experience with medical cannabis as a treatment, with patients who have benefited from its use, and with the practice of family medicine in a patient population that includes persons from a wide variety of backgrounds, age groups and states of health.
My goals are to give patients some ideas about what might be expected from medical cannabis consultation as it would be conducted in my office, and to give clinicians some information about which aspects of the patient’s history, diagnosis and physical condition I consider most relevant in decision making about medical cannabis use.
“Acceptable Standards”
Because medicine is a constantly evolving field, there is a wide range of acceptable standards of care for treating many specific problems. This is more noticeable in dealing with symptom management as opposed to curative therapy; it is particularly relevant in a new field such as Cannabis Therapeutics, in which research has historically been constrained by legal considerations.
In my practice, cannabis is most frequently employed for symptom management (Larson, 1992) as well as for the reduction of what has been termed “symptom distress” -the physical or mental anguish or suffering that results from the symptoms the patient is experiencing (Rhodes & Watson, 1987).
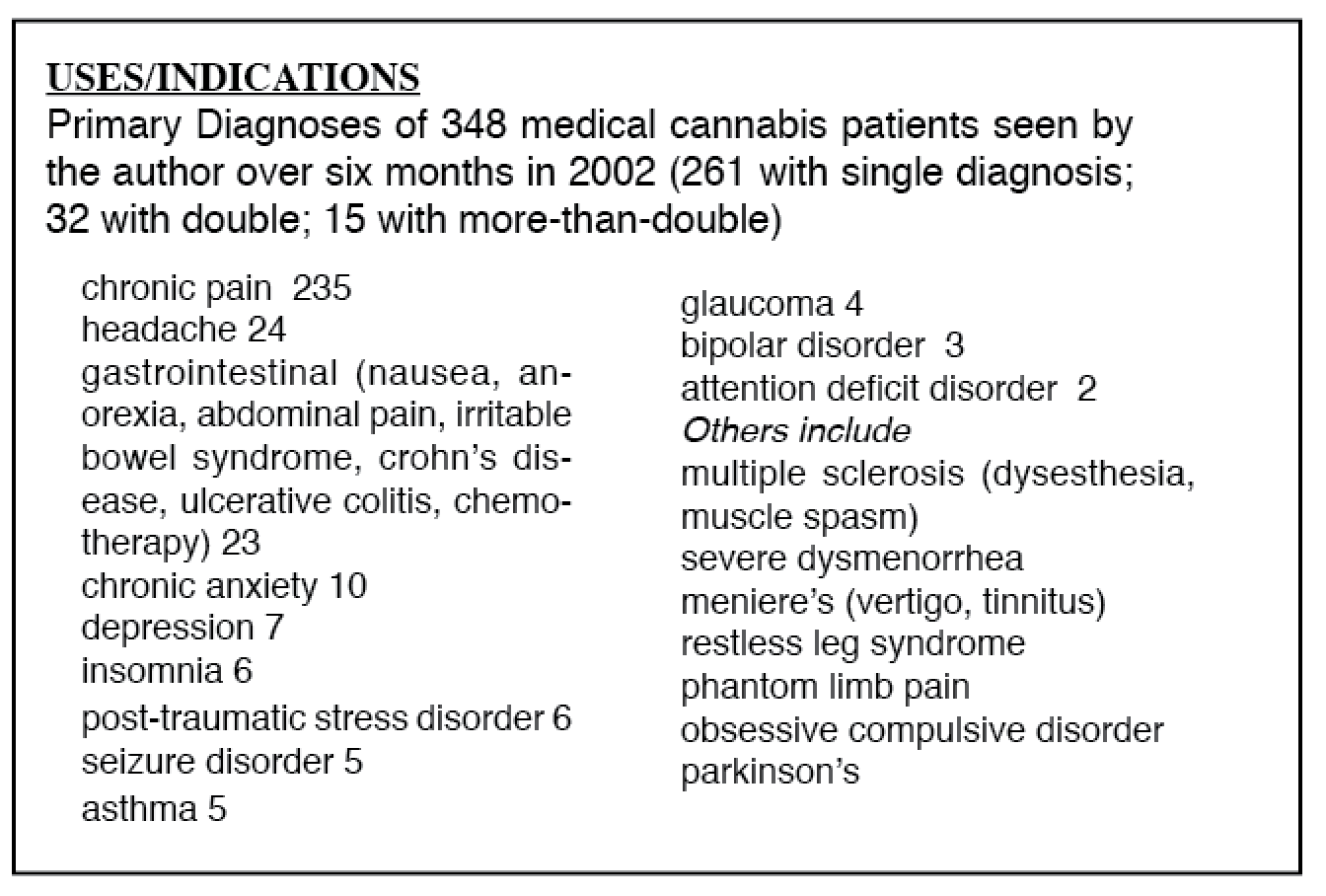
With appropriate use of medical cannabis, many of these patients have been able to reduce or eliminate the use of opiates and other pain pills, Ritalin, tranquilizers, sleeping pills, anti-depressants and other psychiatric medicines, as well as to substitute the use of medical cannabis as a harm reduction measure for specific problematic or abused substances with a much more serious risk profile (including alcohol, heroin/opiates, and cocaine). The diagnoses of my medical cannabis patients (see sidebar below) are consistent with the bulk of my medical practice diagnoses.
Symptoms are subjective phenomena by definition, and as such are difficult to evaluate. Symptoms include, but are not limited to: fatigue, insomnia, depression, anxiety, nausea, vomiting, anorexia, elimination problems, and breathing difficulty.
The control of symptoms and the alleviation of symptom distress are some of the most important therapeutic uses of cannabis. Both the alleviation and the control of symptoms remain areas in which further research is needed (Grant, 1992).
The need for additional research on symptom management is compounded by the lack of research and standards for the use of cannabis therapies. Legal disapprobation, restrictions on the opportunities for clinical research intrinsic to cannabis’ status as a Federal Schedule I Controlled Substance, and a long historic gap in the accumulation of clinical writing on cannabis therapeutics since criminalization in the 1930s have resulted in there being relatively little clinical literature from which we can seek guidance.
The Medical Board of California (MBC) and the California Medical Association (CMA) have a “working group” drafting guidelines, but seven years after the therapeutic use of cannabis was legalized, there are no practice standards other than what is usually expected of any clinician in the course of his or her practice.
“Any physician who recommends the use of marijuana by a patient,” according to the Medical Board’s July 2003 Action Report (restating a 1997 edict), “should have arrived at that decision in accordance with accepted standards of medical responsibility, i.e., history and physical examination of the patient; development of a treatment plan with objectives; provision of informed consent, including discussion of side effects; periodic review of the treatment’s efficacy and, of critical importance, proper record keeping that supports the decision to recommend the use of marijuana. However, the Board recognizes that these principles may require further elaboration to take into account the factors that may affect the physician-patient relationship in this context.”
My Practice and Standards
I have developed (and continue to refine) standards for the recommendation of medical cannabis in my own practice, reflecting my quarter century as a Board certified Family Physician providing primary health care. These are my own standards and should not be construed as criteria for any other physician practicing within the scope of his or her training and license.
General requirements
1. The patient should have a current source of primary care -a Primary Care Provider (PCP)- whom he or she sees regularly.
2. The patient should be seen regularly for the serious illness or symptoms for which medical cannabis is used, by either the PCP or by a specialist, chiropractor, or other health practitioner of the patient’s choice.
These requirements accomplish two important objectives:
• Affirming that the patient has access to primary care.
• Clarifying my role as a consulting physician, and not the primary care practitioner (a common misunderstanding).
Even if the serious illness or symptom is stable, I advise the patient to see his or her physician yearly, to review and update the history and physical.
I generally describe this requirement to the patient by saying: “I don’t want to be the only physician who is aware of your illness or symptom, since I am NOT your primary care practitioner.”
My medical cannabis evaluation is a medical-legal consultation, and is not to be confused with the provision of primary care.
Phone screening
Patients calling for a medical cannabis evaluation are screened by phone to make sure they understand my requirements prior to being given an initial appointment, and to eliminate those who clearly do not qualify.
Pre-appointment
A 45-minute appointment is scheduled for new patients, or 30 minutes for annual re-evaluations. The patient is mailed a detailed questionnaire, along with release forms to obtain records that will be required for the visit.
The patient must fill out the questionnaire in advance of the visit, and must request or bring medical records related to his or her serious illness.
Appointment
The medical cannabis evaluation is conducted in a face-to-face office visit, which includes the collection of relevant history, problem-specific physical exam, and review of the completed questionnaire and outside medical records.
A written summary of the patient’s interview and history is completed for the patient’s chart.
All of these data are assessed for indications that cannabis may be of benefit for the patient’s symptoms or problems.
Pros and cons of medical cannabis use are discussed with the patient, and informed consent documents are reviewed and signed. Patients are advised that they should continue to assess the benefits that they receive from medical cannabis, and should continue its use only if it continues to benefit their symptoms.
Based on all of the above, a decision is reached on whether or not to recommend cannabis to the patient.
Limited approval -for three months or less- may be given in cases where there exists some documentation or physical evidence of a serious illness for which cannabis might be beneficial, but more recent records are required and/or expected to arrive.
Follow-up
Appropriate follow-up appointments are arranged for patients receiving recommendations. Yearly re-evaluation is a minimum.
Our staff is available to help patients complete requests for medical records, and to assist patients in collecting and collating their medical documentation.
More frequent follow-up visits may be required in certain circumstances, such as in some psychiatric diagnoses and some mood disorders, especially if the patient is not receiving ongoing psychiatric care. In this instance, I may require the patient to return with a family member or close friend to corroborate that patient does better with cannabis than without it.
Patients are to continue regular follow-up with the PCP and/or specialist for the serious illness or symptom for which the patient uses cannabis medicinally. At yearly renewal re-evaluation visits, I expect the patient to bring in documentation that his or her primary provider is aware of the serious illness or symptom, and is seeing the patient for re-evaluation at least yearly.
Forms
I have developed the following forms for use in conducting medical cannabis evaluations:
• Consent to assume risk for medical marijuana.
• A questionnaire (adapted from the questionnaire developed by the California Cannabis Research Medical Group).
• Recommendation/approval form.
If a 12-month recommendation is provided, it is dated to expire on the last day of the month, to allow the patient a one-month window to be re-evaluated in their anniversary month. Lately I have embossed the original recommendation with my seal, and added small lettering on certificate that says “original is embossed.” The embossing limits the reproducibiliab of the original. I began doing this after finding that a patient had altered his original certificate. (An extremely rare occurrence.)
Safety
Regarding safety, U.S. Administrative Law Judge Francis L. Young in September, 1988, after reviewing all the evidence on rescheduling cannabis from Schedule I to Schedule II, stated: “In strict medical terms marijuana is far safer than many foods we commonly consume. For example, eating ten raw potatoes can result in a toxic response. By comparison, it is physically impossible to eat enough marijuana to induce death. Marijuana, in its natural form, is one of the safest therapeutically active substances known to man. By any measure of rational analysis marijuana can be safely used within a supervised routine of medical care.”
Limitations
Significant limitations on my discussions with medical cannabis patients are imposed by federal government requirements or threats. For example, I don’t suggest an amount of cannabis to use unless it’s to suggest “less” or a safer method of ingestion for harm reduction/risk minimization purposes.
Experienced medical users will know how to titrate their dosage to achieve the desired effect. In my experience, medical cannabis users consume widely varying amounts. (The handful of patients who remain in the Federal IND program, which supplies cannabis to patients, receive six pounds per year in tinned, pre-rolled cigarette form.)
Nor do I discuss the locations of dispensaries or how to obtain cannabis. If asked, I explain that federal law prohibits my doing so.
Because accurate information is vital to health and patients should always have access to accurate information, I make available a list of resources other than dispensaries through which they can learn more. These include:
• California NORML’s website: http://www.canorml.org/
• Americans for Safe Access 510-486-8083
• The Oakland Cannabis Buyer’s Cooperative 510-832-5346 (which also
provides patients with a photo ID that is easier to carry in one’s wallet than my full-page recommendation form).
I don’t sign any forms from dispensaries, and I don’t sign caregiver forms.
The designation of a caregiver is not a medical decision, but is determined by agreement between the patient and the caregiver, as defined by Health & Safety Code section 11362.5 (Prop 215).
Documentation -Pros and Cons
There is a wide range of acceptable standards in medicine. Some doctors have been criticized for not requiring documentation of diagnosis when they approve cannabis use. Others feel that the requirement creates unnecessary barriers for patients. My arguments for requiring documentation include:
• It is common in other situations in health care.
• It enhances patient protection, both medical, legal and financial.
• It gives me more confidence that, if called upon to do so, I could successfully defend a patient’s appropriate medical use in a court of law.
If law enforcement calls me to verify compliance with Prop 215, I am able to say: “Not only did I assess the patient, but I have independent documentation of the diagnosis for which the patient uses cannabis.”
In most cases, law enforcement officers have been polite and replied something to the effect of: “Thank you, doctor, we just wanted to make sure it was a valid recommendation.”
The following arguments have been made against requiring documentation:
• It is not necessarily consistent with the long tradition in medicine of a trusted doctor/patient relationship.
• It may imply that it is less than acceptable for a doctor to do his or her own evaluation, and determine that cannabis will or won’t benefit a particular patient.
• Records may be unavailable or difficult to obtain. Consider the situation of a patient who suffered a traumatic injury many years ago, and doesn’t have ongoing care for chronic pain. The patient has been self-treating effectively, and now wants to comply with state law. In this situation, the history and physical examination might be enough to make me feel comfortable without further documentation of the diagnosis.
Notes on Confidentiality
Many patients seek out cannabis consultants because they don’t feel comfortable disclosing to their primary care providers doctors that they have been self-medicating with cannabis.
Although I do require that the patient’s primary provider or other appropriate practitioner be aware of, and follow, the serious illness for which cannabis is used, I do not require that the patient disclose his or her medical cannabis use to these providers in all cases. The wording I generally use in explaining this is: “In a perfect world, you should be able to tell your physician everything. But unless, and until the federal government, employers and insurance companies no longer discriminate against medical cannabis users, there is valid reason not to have cannabis mentioned in your medical records.”
I ask the patient to assess whether he or she feels safe in telling their doctor “off the record” that they’re using cannabis medicinally. If the answer is yes, I encourage them to do so. Your own doctor knows you best, and in a perfect world, one should be able to tell his or her doctor everything.
I don’t accept insurance for medical cannabis consultations, nor do I recommend that the patient bill the insurance company, unless the patient is willing to have his/her insurance company see these records.
Special circumstances
Some patient-care situations deserve special mention, as they present unusual complexities or problems.
Should a patient’s medical cannabis use be questioned, some presentations or
diagnoses are particularly likely to be challenged by school, probation or law enforcement authorities.
Psychiatric Patients
Psychiatric diagnoses, particularly if unstable, are likely to raise this kind of “red flag.” In such cases, it is important to have a good history of the efficacy of cannabis for the patient. Approval of the therapist is desirable; next best is a significant other who can attest to the patient’s condition being improved by medical cannabis use.
Minors
The recommendation of medical cannabis use to minors is an area of controversy. As in all of medicine, one must make a risk/benefit assessment.
The developmental needs of adolescents and children suggest that cannabis use should be discouraged, unless, as would be true in a person of any age, the medical benefit obtained outweighs the risk. Recommendations for medical cannabis for minors should be issued conservatively, and evidence of effectiveness should be well-documented, as should be parental consent.
Elders and/or naïve users
Many elders have never been exposed to a social environment in which cannabis is used recreationally. For these patients, as well as for any naïve or first-time user, the psychological effects may be disturbing. The extensive report on medical cannabis prepared by the National Academy of Sciences Institute of Medicine in 1999 suggests that “for some patients -particularly older patients with no previous marijuana experience- the psychological effects are disturbing (p. 4).”
In the years following the legalization of cannabis for medical use, only a small fraction of patients seeking physician approval have been cannabis-naive. At least 90 percent of those seeking approval from CCRMG-affiliated physicians already know that, for them, the benefits outweigh any adverse effects. More naive patients can be expected to inquire about cannabis as a treatment option as favorable research results from Europe are reported in the literature.
How will patients learn to use?
An additional question in relation to the inexperienced user is that of how the patient will learn to use cannabis.
Who is available to teach the patient?
Will an informed, experienced user be available when the patient first tries medical cannabis?
In what form will the patient ingest cannabis?
Does he or she understand the concept of titration of the dose?
Is there a protected environment available to the patient for his or her initial and subsequent use?
How should the patient be counseled about the possibility of unwanted effects?
What precautions or preparation should the patient be advised to use?
Conclusions
Physicians who are considering whether to approve cannabis use by their patients must first educate themselves on the subject. Cannabis has a long, impressive history as a safe and effective medicine. Although the United States has limited studies on the benefits of cannabis, the National Institute on Drug Abuse has funded significant research into its mechanism of action. Universities and major pharmacuetical companies are conducting groundbreaking studies. Much of this research is available in: Grotenhermen and Russo:”Cannabis and Cannabinoids: Pharmacology, Toxicology, and Therapeutic Potential.”
My advice to colleagues, in brief:
• Practice responsible medicine, including encouraging patients to obtain appropriate follow-up of their illnesses from their primary care practitioner.
• Maintain good documentation, both of previous history and outside records,
and of your own history, physical, assessment, and follow-up plan.
• Be able to explain your decision-making process in a court of law should you be called upon to support a legitimate patient, or to discuss a patient’s cannabis use with an employee health clinician. On occasion, a question may arise as to whether a patient can perform safety-sensitive functions in the workplace. It may be important to document that the patient does not use cannabis in a specified time frame in relation to hours of work.
• Do not assist anyone in breaking the law. The vast majority of medical cannabis patients are honest and appropriate medical users under California law . (Notwithstanding the situations in which doctors have had visits from undercover agents posing as patients).
I find cannabis patients to be, on the whole, as honest and forthright as patients or people in general.
It should go without saying, but I will say it: No matter how convinced you may be of the relative benign-ness of cannabis, do not agree to do anything illegal. Undercover agents have been known to say to a doctor: “I don’t have an illness, I just want to be able to smoke marijuana.” It should be clear that this is not a legitimate use of the Compassionate Use Act .
There are millions of real patients to help.
Office Setting
My office is close to the University of California campus in a lovely 60-year-old brick medical-dental building in Berkeley that reminds me of the medical buildings I went to when I was a kid in Michigan in the ’50’s. There is a small garden behind the office and a generally welcoming and calm atmosphere, surrounded by the bustling activity of a busy academic community. We share the office building with a dental practice, and there are persons of all ages, backgrounds and walks of life in our waiting room. We have a multi-cultural staff, and several languages are spoken in the office.
Dr. Lucido can be contacted at drfrank@drlucido.com or 510-848-0958.
References
Goldberg, C. (2002a, 8/28/03). A few thoughts. University of California, Davis School of Medicine. Retrieved November 26, 2003, from:
http://medicine.ucsd.edu/clinicalmed
Goldberg, C. (2002b, 8/28/03). A practical guide to clinical medicine: Outpatient clinics [website]. University of San Diego School of Medicine.
Retrieved November 24, 2003, from: http://medicine.ucsd.edu/clinicalmed/clinic.htm
Grant, M. (1992). Future directions in symptom management. In P. Larson (Ed.), Symptom management proceedings. San Francisco: UCSF Nursing Press.
Grotenhermen, F. & and E. Russo (2002) Cannabis and cannabinoids, Pharmacology, toxicology, and therapeutic potential. Binghanton, NY Haworth Press www.haworthprsss.com
Institute of Medicine (1999) Marijuana and medicine: Assessing the science base. Washington D. C., National Academy Press
Larson, P. (1992). Symptom management procedings. Paper presented at the Symptom management: Research trajectories and practice implications, San Francisco.
Rhodes, V., & Watson, P. (1987). Symptom distress -the concept, past and current. Seminars in Oncology Nursing, 3(4), 242-247.
Full Disclosure
I am one of approximately nine physicians who have been investigated by the Medical Board of California in relation to recommending medical cannabis. My strong belief that I was practicing the highest standards of medicine provided a level of comfort and confidence that I would not have expected to maintain during such a stressful, time-consuming ordeal.
I was also reassured by having good legal counsel and the support of many fellow physicians, as well as my patients, family, and friends. In August, 2003, one year after I was served a subpoena to appear at a Medical Board hearing, I was effectively exonerated.
Regrettably, my experience with the Board has been shared by a number of other responsible physicians who were also inappropriately targeted for investigation for having recommended medical cannabis.
The complaints triggering these investgations have not come from patients or caregivers, but from officials in various branches of law enforcement. The few exceptions include a complaint from a spouse in the midst of a bitter divorce, and a complaint from a high school principal.