Viewpoint: “Evolution of Continuing Medical Education: Promoting Innovation Through Regulatory Alignment”
By Graham T. McMahon, MD, MMSc, Accreditation Council for Continuing Medical Education (gmcmahon @accme.org) and Susan E. Skochelak, MD
Physicians thrive personally and provide better care when they are working in a supportive environment.1 There is a need to create a system in which physicians find effective and efficient education that not only augments their ability to deliver optimal care, but also provides intellectual stimulation and fosters personal growth. Top-down mandates for education are not only typically ineffective, but create cynicism that erodes clinicians’ trust and engagement in their continuing medical education (CME).
Clinicians Expect More From CME
Currently, the framework for CME is managed through a collaboration between the Accreditation Council for Continuing Medical Education (ACCME) and the American Medical Association (AMA). The ACCME serves as the national accreditor and sets the standards for entities and organizations that provide education, such as health systems, schools, and professional societies, which, when accredited, can issue the AMA PRA Category 1 Credit. The AMA establishes the standards for the credit system that is used by physicians to demonstrate engagement in professional self-development to groups such as state licensing boards, hospitals, and insurers.
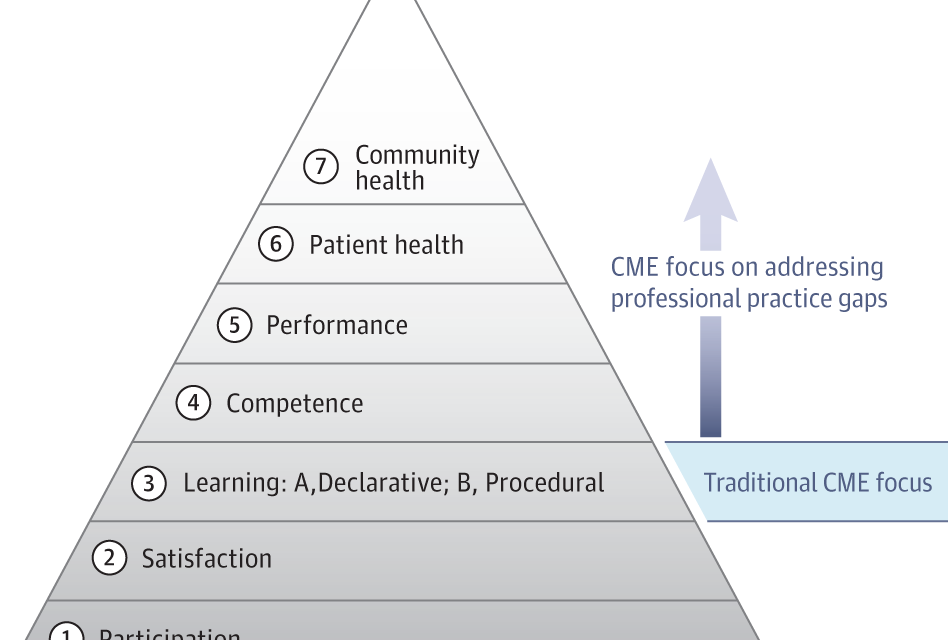
Each of these organizations seeks to support clinicians and the development of learning opportunities. Those expectations for learning continue to evolve: in a world in which physicians can learn about new guidelines more quickly by retrieving them on a handheld device than by listening to a lecture, the traditional formats of information transfer that used to be the primary currency of education have diminishing value. Older models of educational delivery, such as passive listening in large groups, can be inefficient, ineffective, and reinforce a mistaken belief that being present means that learning is occurring.
Rather than gathering for informational updates, most physicians now seek opportunities to convene to practice skills, receive feedback, glean wisdom, and interact. Today’s learners increasingly and appropriately expect their education to be professionally delivered, tailored to their needs and their practice environment, and support process and quality improvement. As adult learners, physicians increasingly seek learning programs that are adaptable to their learning style and accessible where they live, learn, and practice. From bedside learning to learning from teaching, physicians should be able to integrate their daily activities into a CME portfolio.
Momentum for Change
The ACCME and AMA want to ensure that the education community has the permission it needs to deliver on those changing expectations. To move CME programs forward, educators need the capacity and support to create active, dynamic, and participatory learn- ing. These organizations have a responsibility to advance the field by encouraging educators to implement best practices in pedagogy, engagement, evaluation, and change management, and to focus on generating meaningful outcomes. The goal of this effort has been to ensure that wherever learning is happening, CME is there.
Toward that end, leadership, staff, and volunteers at the AMA and ACCME collaborated on a strategy to more closely align the 2 organizations’ requirements, simplify the system, and eliminate any barriers (perceived or real) that would constrain innovation in educational delivery. To develop their approach, the organizations convened listening sessions with various groups (including staff, volunteers, and leadership from accredited organizations and state medical societies), gathering feedback from physicians and educators about how to reconstruct the system to better support the evolution of CME. Based on this feedback, a joint construct has been created for addressing those objectives, and a call for comment was issued. More than 90% of the 170 organizations and individuals who responded to the joint survey strongly endorsed the proposal and agreed that it would give them sufficient opportunity to innovate and evolve their CME programs. The proposal was subsequently adopted by the AMA2 and ACCME3 and went into effect in September 2017.
Fewer Requirements, More Options
This recently announced alignment reduces burdens on educators by providing a unified set of rules. The construct preserves the integrity of professional self-regulation and relies on 7 core requirements that ex- press principles for education excellence and independence from commercial influence. The core requirements represent an alignment of AMA and ACCME values and do not introduce any new rules for accredited CME providers. As a further simplification, the alignment has been integrated into the existing accredita- tion and reaccreditation processes so that accredited CME providers that demonstrate compliance with ACCME requirements are deemed to have met the AMA core requirements.
As part of the alignment, the AMA simplified and reduced its learning format requirements. There were previously specific requirements for 7 formats; now, there are specific requirements for only 3 formats: enduring materials, journal-based CME, and performance improvement CME. In addition, the requirements for these 3 format types were simplified, so that learning is pri- oritized. For example, the familiar posttests can be replaced with a self-reflective statement about what has
Examples of Educational Approaches That Are Now Acceptable for Continuing Medical Education Activities
• Hybrid/blended learning (eg, recorded webinar followed by in-person, small-group problem-solving sessions; live webcast followed by a group quality improvement effort)
• Bedside case discussions
• Review of records and registry data by a physician or group Use of art to stimulate reflections about personal wellness Online case discussion using social media
• Procedural training using virtual reality
• Role-play simulation to practice communication skills Interactive game to learn effective practice management
been learned and how the learner plans to change; the outcome measure for a quality improvement effort can be locally determined.
One of the most important features of the alignment is the creation of an “other” format category that educators can use to designate an activity if it does not fall into an established category. Instead of focusing on how to construct an activity to fit within a previously regulated format, educators now have the freedom to customize the best approach for their learners using a variety of models and can more readily apply innovative education strategies. With this new category, educators are empowered to use blended or new approaches to drive toward meaningful learning and change without needing to seek preapproval. Educators are free to deploy new technologies, such as simulation, adaptive e-learning, virtual reality, gamification (ie, applying game-playing elements [eg, point scoring] to other areas, such as learning), and social media, into their medical education approaches, to cite just a few examples (Box). Information learned about the effectiveness of these evolved formats will be shared with the educational community to promote the adoption of best practices.
Future Directions
Simplification, permission, and encouragement will only be meaningful if educators and educational groups take advantage of these opportunities to evolve their approach to and use of CME. Physicians too must be prepared and willing to engage in the types of evolved educational activities that require active participation and are intellectually challenging. More effective educational program- ming will be self-reinforcing: health system leadership will increasingly fund programming that contributes to meaningful practice transformation. Innovative educational approaches will be a key resource in the development of learning health systems, which, as defined by the National Academy of Medicine,5 promote continuous improvement and innovation by aligning science, informatics, incentives, and culture; embed best practices in the delivery process; and capture new knowledge as an integral byproduct of the delivery experience. With more flexibility to define educational methods, CME educators can increasingly support intellectual fulfill- ment of clinicians and help restore joy in practice, relieve physicians of administrative burden, sustain functional interprofessional teams, and effect meaningful improvements in the quality and safety of patient care.6
To deliver high-quality team care, teams need to learn to- gether. In their governance role, accreditors have the opportunity to promote interprofessional continuing education that improves team-based care. The ACCME, in collaboration with the Accreditation Council for Pharmacy Education and the American Nurses Credentialing Center, created the first joint accreditation system to facilitate interprofessional continuing education. This program can serve as a model for accreditors in the health professions for developing systems that promote and facilitate team-based education by removing barriers between professions and expanding the delivery of interprofessional continuing education to facilitate measurable improvements in team performance.7
Regulatory requirements that facilitate choice and accommodate differences will enable health system leaders, educators, and learners to meet the diverse and changing needs of the health care environment. As regulators, the AMA and ACCME expect educators to design programs based on needs assessments and practice gaps and to continuously evaluate and improve their offerings. These organizations accept the obligation to similarly evolve with the community. Success will mean identifying needs and gaps in CME, relinquishing some of the methods that have served regulators in the past, and adopting a variety of new approaches that reflect the same innovative spirit and nimbleness that is expected of educational providers. With a new vision of the role of regulators, credit and accreditation systems can collaboratively create frameworks that inspire and nurture the community of educators, empowering them to achieve their full potential and deliver education that makes a difference for physicians and patients. In providing this permission, encouragement, and support, the hope is that everyone— clinicians, patients, communities, and health systems—will benefit.
Published Online: January 22, 2018. doi:10.1001/jama.2017.19954
Conflict of Interest Disclosures: Both authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr McMahon is a salaried employee of the Accreditation Council for Continuing Medical Education. Dr Skochelak is the group
vice president for medical education at the American Medical Association.
REFERENCES
1. ShanafeltTD,MungoM,SchmitgenJ,etal. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016;91 (4):422-431.
2. American Medical Association. AMA/ACCME alignment. https://www.ama-assn.org/education /ama-pra-credit-system. Accessed
November 22, 2017.
3. Accreditation Council for Continuing Medical Education. AMA/ACCME alignment. http://www .accme.org/cme-providers/ama-accme-alignment. Accessed November 22, 2017.
4. Accreditation Council for Continuing Medical Education. Standards for commercial support. http://www.accme.org/requirements /accreditation-requirements-cme-providers
(Reprinted)
/standards-for-commercial-support. Accessed November 22, 2017.
5. National Academy of Medicine. The learning health system series. https://nam.edu/programs /value-science-driven-health-care/learning-health -system-series/. Accessed November 22, 2017.
6. McMahon GT. The leadership case for investing in continuing professional development. Acad Med. 2017;92(8):1075-1077.
7. JointAccreditationforInterprofessional Continuing Education. By the team for the team. http://www.jointaccreditation.org/sites/default /files/2016_Joint_Accreditation_Leadership_Summit _Report_0.pdf. Accessed November 22, 2017.
© 2018 American Medical Association. All rights reserved.
Downloaded by Fred Gardner on 01/22/2018