Did you hear that under new Guidelines from heart specialists, “Millions More Americans Will Need to Lower Blood Pressure?” (Nodding to audience) That’s what the headline said. For many years my doctor insisted that I go on blood pressure meds. I would promise to get more exercise. I meant it —but exercise is hard to get. After six or seven years, I finally relented and he was pleased. He said he would put me on WHAT BRAND, but when he saw that my insurance didn’t cover it, he said “Lisinopril is just as good.” When 20mg didn’t help, he doubled the dose. And finally my numbers did get down to around 140-over-90, which was borderline acceptable to him, which was a relief to me. I stopped taking my blood pressure —as if it was a game of blackjack and I could hold.
Now the Experts have lowered the cut-off point to 130 over 80. Which means I have high blood pressure. Again. Also, a bad case of Sisyphus.
Drum roll, please.
The American Heart Association and the American College of Cardiology proposed the new guidelines, according to Gina Kolata’s story in the New York Times. The number of US adults who qualify for a high-blood-pressure diagnosis instantly rose from 72 million to 103 million. Personally, I’m committed to getting more exercise.
N of 1 Trial
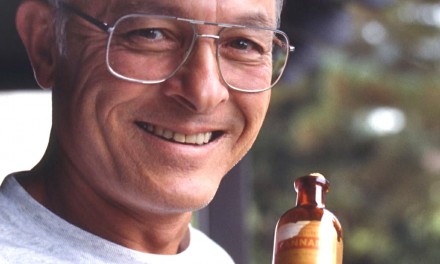
I emailed the above item to my doctor who wanted to know my current blood pressure. (Dr. Deutsch has a good sense of humor, plus he’s always in a hurry.) So I found the Tensiometro and my numbers turned out be 155 over 94— high even under the old guidelines. I rationalized that I’d just had a strong cup of freshly ground Peet’s Major Dickinson. Then, since my sleeve was rolled up and the Tensiometro on the table, I decided to test the effect of cannabis —specifically, a chemovar called “Cookie Batter” developed by Napro Research. After three tokes, my blood pressure had dropped to 134/76! This is the lightest-weight piece of anecdotal evidence you’ll ever hear, but I can’t wait to tell Dr. Deutsch. And, of course, more research is needed.
Dr. Welch Responds to Kolata Piece
An excellent op-ed in the November 16 New York Times by H. Gilbert Welch, a professor of medicine at the Dartmouth Institute for Health Policy and Clinical Practice responds to the redefining of blood pressure standards as reported by Gina Kolata. (This is why we don’t cancel the print edition and call our column “Bad Times and Good.”)
Welch explains:
The new recommendation is principally in response to the results of a large, federally funded study called Sprint that was published in 2015 in The New England Journal of Medicine. Sprint was a high-quality, well-done study. It randomly assigned high blood pressure patients age 50 and older to one of two treatment targets: systolic blood pressure of less than 140 or one of less than 120. The primary finding was that the lower target led to a 25 percent reduction in cardiovascular events — the combined rate of heart attacks, strokes, heart failures and cardiovascular deaths.
Relative changes — like a 25 percent reduction — always sound impressive. Relative changes, however, need to be put in perspective; the underlying numbers are important. Consider the patients in Sprint’s high target group (less than 140): About 8 percent had one of these cardiovascular events over four years. The corresponding number in the low target group (less than 120) was around 6 percent. Eight percent versus 6 percent. That’s your 25 percent reduction…
One of the most impressive findings in Sprint was that few patients had problems with low blood pressure like becoming lightheaded from overmedication and then falling. But one of the most important principles in medicine is that the effects seen in a meticulously managed randomized trial may not be replicated in the messy world of actual clinical practice.
Serious falls are common among older adults. In the real world, will a nationwide target of 130, and the side effects of medication lowering blood pressure, lead to more hip fractures? Ask your doctors. See what they think.
Let me be clear: Using medications to lower very high blood pressure is the most important preventive intervention we doctors do. But more medications and lower blood pressures are not always better for everyone.
I suspect many primary-care practitioners will want to ignore this new target. They understand the downsides of the relentless expansion of medical care into the lives of more people. At the same time, I fear many will be coerced into compliance as the health care industry’s middle management translates the 130 target into a measure of physician performance. That will push doctors to meet the target using whatever means necessary — and that usually means more medications.
So focusing on the number 130 not only will involve millions of people but also will involve millions of new prescriptions and millions of dollars. And it will further distract doctors and their patients from activities that aren’t easily measured by numbers, yet are more important to health — real food, regular movement and finding meaning in life. These matter whatever your blood pressure is.